Intro: Venous thromboembolism (VTE) is a common cause of death among cancer patients, second only to cancer progression. Identifying factors predicting worse outcomes among cancer patients with VTE would be useful clinically. For cancer patients with pulmonary emboli (PE), it remains unclear whether concomitant leg deep vein thrombosis (DVT) as a source for further embolization adversely impacts this risk. The aim of this project was to determine the impact of residual DVT on adverse outcomes among cancer patients suffering acute PE.
Methods: Consecutive patients with confirmed acute PE (March 1, 2013 - June 30, 2021) underwent ultrasound (US) imaging and were divided into two groups depending on the presence or absence of leg DVT. PE severity was classified based on AHA criteria. Patients were followed prospectively for VTE recurrence, major and clinically relevant non-major bleeding (CRNMB) and all-cause mortality.
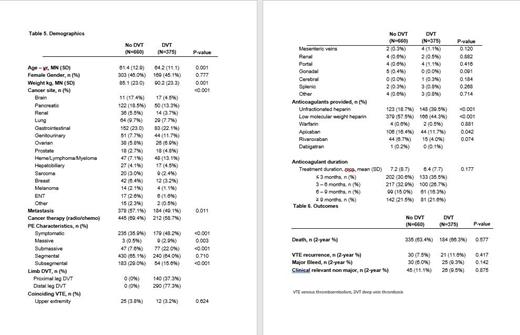
Results: Over the study interval, 1,035 cancer patients with PE were enrolled (Table 1). Of these, 375 (36.2%) had leg DVT confirmed by US. Patients with leg DVT were older (64.2 vs 61.4 years, p = 0.01), heavier (90.2 vs 85.1 kg, p <0.001), with lower metastatic disease prevalence (49.1% vs 57.1%, p = 0.01) compared to those without leg DVT. Cancer type distribution also differed between groups. PE patients with DVT more often had prostate, genitourinary, and hematologic cancers while those without DVT more often had pancreatic and breast cancers. Patients with DVT more often had symptomatic PE (48.2% vs. 35.9%, p < 0.001), massive (2.9% vs 0.5%, p < 0.001), and submassive (22.0% vs 7.6%, p < 0.001). Patients with DVT more often received unfractionated heparin (39.5% vs 18.7%, p < 0.001) whereas those without DVT were more frequently treated with low molecular weight heparin (57.5% vs. 44.3%, p <0.001), and apixaban (16.4% vs. 11.7%, p < 0.05). Anticoagulant duration, VTE recurrence, major bleeding and CRNMB were similar between groups (Table 2).
Conclusion: Among a large cohort of cancer patients with pulmonary emboli, significant clinical and cancer specific differences exist comparing those with and without leg DVT.While theoretically increasing the risk of recurrent embolization, the presence of residual DVT does not appear to adversely impact important outcomes among cancer patients adequately treated with anticoagulation.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal